Irregularly irregular rhythm, rate 60 beats/min. Image courtesy of Dr Podrid. The QRS complexes have a normal duration (0.10 sec) and axis between 0° and +90° (positive QRS complex in leads I. Sinus arrhythmia: There is a cyclical acceleration of heart rate with inspiration and slowing with expiration. The beat to beat interval is slightly different.The rhythm is regularly irregular, in the sense that there is a pattern to irregularity. This is termed sinus arrhythmia. This can lead to a rapid or irregular heartbeat, along with symptoms like an increased appetite and sudden weight loss. That said, experiencing them regularly is not. “If heart palpitations. Atrial fibrillation is an irregular and often rapid heartbeat caused by chaotic electrical activity in the heart's upper chambers. Supraventricular tachycardia is a faster-than-normal heart rate (tachycardia means fast heart rate) that begins above the heart's lower chambers. Both of these may cause palpitations that may be brief or prolonged. Regularly irregular. Pulse seems to miss a beat with a definite pattern. Heart organ disharmony or exhaustion of the organs: Knotted: Irregularly irregular and slow. Pulse seems to miss a beat with no apparent pattern. Cold obstructing the flow of qi and blood. Short: Pulse doesn't seem to fill all three positions (front, middle, rear).
- Regularly Irregular Pulse Rhythm
- Irregular Pulse Rate
- Regular Irregular Pulse
- Regularly Irregular Pulse
- Irregular Pulse Interval
Having a hiccup in your heart rhythm can be uncomfortable – as well as frightening. But when does an extra heartbeat or other unexpected feeling warrant a visit to your doctor?
John Hummel, MD, a heart rhythm specialist at the Richard M. Ross Heart Hospital, sheds some light on irregular heart rhythms, which are fairly common.
“It can be tempting to jump to the worst-case scenario when it comes to your heart, and to think that an irregular heartbeat is a sign of a serious disease,” says Dr. Hummel. “But it doesn't always require treatment.”
The possible causes of an irregular heartbeat can vary widely – from too much caffeine to a more potentially dangerous condition of having your blood pressure skyrocket or plummet.
There are several types of irregular heartbeats. Dr. Hummel explains some people experience an extra heartbeat, a skipped beat, too fast of a beat (called tachycardia) or too slow of a beat (called bradycardia).
When to see a doctor immediately?
Dr. Hummel says it can be difficult for most people to know if an irregular heartbeat is a sign of something more serious.
Go immediately if you have additional symptoms with your irregular heartbeat or you’ve had a heart attack or other heart stress. According to Dr. Hummel, those symptoms include fainting, dizziness, chest pain, swelling in your leg or shortness of breath.
“There’s a big difference between sitting in a chair and noticing your heart skipping and having fluttering that makes you feel like I’m going to pass out,” says Dr. Hummel.
“The other issue is whether your heart is structurally normal. If it’s not, abnormal heart rhythms more commonly will increase your risk of stroke or sudden death.”
Look at your actions and environment
Dr. Hummel says external factors could be causing disruptions in your heart rhythm:
- Too much caffeine or alcohol
- Dehydration
- Drug abuse
- Fever
- Anemia
- Emotional distress
- Sleep apnea
- Pregnancy
- Eating or exercising
Dr. Hummel advises you make notes of when you experience irregular heartbeats and share this information with your doctor. Remember, not all unusual heart rhythms will require treatment. 'Abnormal heartbeats can come and go, especially in young people,” states Dr. Hummel.
What type of tests can help diagnose an irregular heartbeat?
The first test is usually an echocardiogram, which looks at the structure and function of your heart. You may have an exercise stress test on a treadmill or stationary bike to measure your heart’s response to exertion. Patients might also be asked to wear a portable monitoring device (called a Holter monitor) for 24 to 48 hours that records every heartbeat and monitors for irregular heart rhythm.
“We have a wide range of diagnostic tools and we work to figure out what the cause is by looking at your actions and your medical history,” explains Dr. Hummel. He points out some people may have an inherited abnormal heart rhythm. Learn more about genetic heart testing.
The bottom line on your irregular heartbeat
- If you have skipped heartbeats, you need to pay attention to your body and then get an assessment.
- The urgency of that assessment is determined by whether you have additional symptoms or structural heart disease.
Overview
What is an arrhythmia?
An arrhythmia (also called dysrhythmia) is an irregular or abnormal heartbeat.
What is my pulse?
Your pulse indicates your heart rate, or the number of times your heart beats in one minute. Pulse rates vary from person to person. Your pulse is slower when you are at rest and increases when you exercise, since more oxygen- rich blood is needed by the body during exercise.
How do I take my pulse?
You can tell how fast your heart is beating by feeling your pulse. You can feel your pulse on your wrist or neck. Place the tips of your index and middle fingers on the inner wrist of your other arm, just below the base of your thumb. Or, place the tips of your index and middle fingers on your lower neck, on either side of your windpipe. Press lightly with your fingers until you feel the blood pulsing beneath your fingers. You may need to move your fingers around slightly up or down until you feel the pulsing.
You can count the number of beats in 10 seconds and multiply by 6 to determine your heart rate in beats per minute. A normal heart rate, at rest, is 50 to 100 beats per minute.
Your Heart Rate: Pulse in 10 seconds x 6 =_
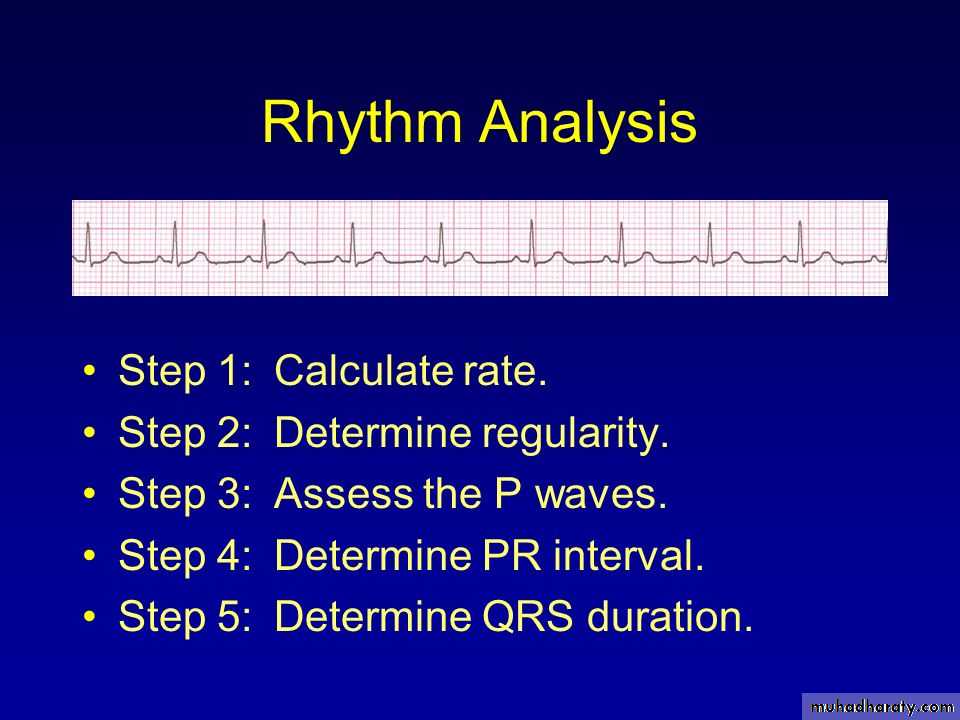
Heart Rhythms on ECG
The heart’s electrical system triggers the heartbeat. Each beat of the heart is represented on the electrocardiogram (EKG or ECG) by a wave arm.
The normal heart rhythm (normal sinus rhythm) shows the electrical activity in the heart is following the normal pathway. The rhythm is regular and the node is normal (about 50 to 100 beats per minute).
Tachycardia: fast heart rhythm (greater than 100 beats per minute)
Bradycardia: slow heart rhythm (less than 60 beats per minute)
The Heart’s Electrical System
The atria (the heart’s upper chambers) and ventricles (the heart’s lower chambers) work together, alternately contracting and relaxing to pump blood through the heart. The electrical system of the heart is the power source that makes this possible. Here’s what happens during a normal heartbeat:

Irregular heart rhythms can also occur in normal, healthy hearts. Arrhythmias can also be caused by certain substances or medications, such as caffeine, nicotine, alcohol, cocaine, inhaled aerosols, diet pills, and cough and cold remedies. Emotional states such as shock, fright or stress can also cause irregular heart rhythms.
Arrhythmias that are recurrent or related to an underlying heart condition are more concerning and should always be evaluated by a doctor.
In most cases, treating the underlying condition will take care of the arrhythmia. If not, many medications and procedures are available to eliminate or control the abnormal heart rhythm.
What are the types of arrhythmias?
- Tachycardia: A fast heart rhythm with a rate of more than 100 beats per minute.
- Bradycardia: A slow heart rhythm with a rate below 60 beats per minute.
- Supraventricular arrhythmias: Arrhythmias that begin in the atria (the heart’s upper chambers). “Supra” means above; “ventricular” refers to the lower chambers of the heart, or ventricles.
- Ventricular arrhythmias: Arrhythmias that begin in the ventricles (the heart’s lower chambers).
- Bradyarrhythmias: Slow heart rhythms that may be caused by disease in the heart’s conduction system, such as the sinoatrial (SA) node, atrioventricular (AV) node or HIS-Purkinje network.
Types of Supraventricular Arrhythmias
Supraventricular arrhythmias begin in the atria
Types of supraventricular arrhythmias include:
Premature atrial contractions (PACs)
Early, extra heartbeats that originate in the atria.
Paroxysmal supraventricular tachycardia (PSVT)
A rapid but regular heart rhythm that comes from the atria. This type of arrhythmia begins and ends suddenly.
Accessory pathway tachycardias (bypass tract tachycardias)
A fast heart rhythm caused by an extra, abnormal electrical pathway or connection between the atria and ventricles. The impulses travel through the extra pathways as well as the usual route. This allows the impulses to travel around the heart very quickly, causing the heart to beat unusually fast (example: Wolff- Parkinson-White syndrome).
AV nodal re-entrant tachycardia (AVNRT)
A fast heart rhythm caused by the presence of more than one pathway through the atrioventricular (AV) node.
Atrial tachycardia
A rapid heart rhythm that originates in the atria.
Atrial fibrillation
A very common irregular heart rhythm. Many impulses begin and spread through the atria, competing for a chance to travel through the AV node. The resulting rhythm is disorganized, rapid and irregular. Because the impulses are traveling through the atria in a disorderly fashion, there is a loss of coordinated atrial contraction.
Regularly Irregular Pulse Rhythm
- Learn more about atrial fibrillation.
Atrial flutter
An atrial arrhythmia caused by one or more rapid circuits in the atrium. Atrial flutter is usually more organized and regular than atrial fibrillation.
Types of Ventricular Arrhythmias
A ventricular arrhythmia begins in the heart’s ventricles.
Types of ventricular arrhythmias include:
Premature ventricular contractions (PVCs)
Early, extra heartbeats that originate in the ventricles. Most of the time, PVCs don’t cause any symptoms or require treatment. This type of arrhythmia is common and can be related to stress, too much caffeine or nicotine, or exercise. They can be also be caused by heart disease or electrolyte imbalance. People who have several PVCs and/or symptoms associated with them should be evaluated by a cardiologist (heart doctor).
- Learn more about premature ventricular contractions.
Ventricular tachycardia (V-tach)
A rapid heartbeat that originates in the ventricles. The rapid rhythm keeps the heart from adequately filling with blood, and less blood is able to pump through the body. V-tach can be serious, especially in people with heart disease, and may be associated with more symptoms than other types of arrhythmia. A cardiologist should evaluate this condition.
Ventricular fibrillation (V-fib)
An erratic, disorganized firing of impulses from the ventricles. The ventricles quiver and cannot generate an effective contraction, which results in a lack of blood being delivered to the body. This is a medical emergency that must be treated with cardiopulmonary resuscitation (CPR) and defibrillation (delivery of an energy shock to the heart muscle to restore a normal rhythm) as soon as possible.
- Learn more about sudden cardiac death.
Long QT
The QT interval is the area on the ECG that represents the time it takes for the heart muscle to contract and then recover, or for the electrical impulse to fire and then recharge. When the QT interval is longer than normal, it increases the risk for “torsade de pointes,” a life-threatening form of ventricular tachycardia.
Types of Bradyarrhythmias
A bradyarrhythmia is a slow heart rhythm that is usually caused by disease in the heart’s conduction system. Types of bradyarrhythmias include:
Sinus node dysfunction
Slow heart rhythms due to an abnormal SA node.
Heart block
A delay or complete block of the electrical impulse as it travels from the sinus node to the ventricles. The level of the block or delay may occur in the AV node or HIS-Purkinje system. The heartbeat may be irregular and slow.
Symptoms and Causes
What are the symptoms of an arrhythmia?
An arrhythmia may be “silent” and not cause any symptoms. A doctor can detect an irregular heartbeat during an examination by taking your pulse, listening to your heart or by performing diagnostic tests. If symptoms occur, they may include:
- Palpitations: A feeling of skipped heartbeats, fluttering, 'flip-flops' or feeling that the heart is 'running away'
- Pounding in the chest
- Dizziness or feeling lightheaded
- Shortness of breath
- Chest discomfort
- Weakness or fatigue (feeling very tired)
What causes arrhythmias?
Arrhythmias can be caused by:
- Coronary artery disease
- High blood pressure
- Changes in the heart muscle (cardiomyopathy)
- Valve disorders
- Electrolyte imbalances in the blood, such as sodium or potassium
- Injury from a heart attack
- The healing process after heart surgery
- Other medical conditions
Diagnosis and Tests
How is an arrhythmia diagnosed?
If you have symptoms of an arrhythmia, you should make an appointment with a cardiologist. You may want to see an electrophysiologist — a cardiologist who has additional specialized training in the diagnosis and treatment of heart rhythm disorders.After evaluating your symptoms and performing a physical examination, the cardiologist may perform a variety of diagnostic tests to help confirm the presence of an arrhythmia and indicate its causes.Some tests that may be done to confirm the presence of an irregular heart rhythm include:
- Electrocardiogram (ECG or EKG): A picture of the electrical impulses traveling through the heart muscle. An ECG is recorded on graph paper, through the use of electrodes (small, sticky patches) that are attached to your skin on the chest, arms and legs.
- Ambulatory monitors, such as:
- Stress test: A test used to record arrhythmias that start or are worsened with exercise. This test also may be helpful in determining if there is underlying heart disease or coronary artery disease associated with an arrhythmia.
- Echocardiogram: A type of ultrasound used to provide a view of the heart to determine if there is heart muscle or valve disease that may be causing an arrhythmia. This test may be performed at rest or with activity.
- Cardiac catheterization: Using a local anesthetic, a catheter (small, hollow, flexible tube) is inserted into a blood vessel and guided to the heart with the help of an X-ray machine. A contrast dye is injected through the catheter so X-ray movies of your coronary arteries, heart chambers and valves may be taken. This test helps your doctor determine if the cause of an arrhythmia is coronary artery disease. This test also provides information about how well your heart muscle and valves are working.
- Electrophysiology study (EPS): A special heart catheterization that evaluates your heart’s electrical system. Catheters are inserted into your heart to record the electrical activity. The EPS is used to find the cause of the abnormal rhythm and determine the best treatment for you. During the test, the arrhythmia can be safely reproduced and terminated.
- Tilt table test (also called a passive head-up tilt test or head upright tilt test): Records your blood pressure and heart rate on a minute-by-minute basis while the table is tilted in a head-up position at different levels. The test results may be used to evaluate heart rhythm, blood pressure and sometimes other measurements as you change position.
Management and Treatment
How is an arrhythmia treated?
Treatment depends on the type and severity of your arrhythmia. In some cases, no treatment is necessary. Treatment options include medications, lifestyle changes, invasive therapies, electrical devices or surgery.
Medications
Antiarrhythmic drugs are medications used to convert the arrhythmia to a normal sinus rhythm or to prevent an arrhythmia. Other medications may include heart rate-control drugs and anticoagulant or antiplatelet drugs such as warfarin (a “blood thinner”) or aspirin, which reduce your risk of stroke or developing blood clots.It is important that you know the names of your medications, why they are prescribed, how often and at what times to take them, what side effects may occur, and what medications you have previously taken for your arrhythmia.
Lifestyle changes
Airrhythmias may be related to certain lifestyle factors. The following tips can help limit the occurrence of arrhythmias:
- If you smoke, stop.
- Limit your intake of alcohol.
- Limit or stop using caffeine. Some people are sensitive to caffeine and may notice more symptoms when using caffeinated products, such as tea, coffee, colas and some over-the- counter medications.
- Avoid using stimulants. Beware of stimulants used in cough and cold medications and herbal or nutritional supplements. Some of these substances contain ingredients that cause irregular heart rhythms. Read the label and ask your doctor or pharmacist which medication is best for you.
- Your family may also want to be involved in your care by learning to recognize your symptoms and how to start CPR if needed.
- If you notice that your irregular heart rhythm occurs more often with certain activities, you should avoid them.
Invasive therapies
Electrical cardioversion and catheter ablation are invasive therapies used to treat or eliminate irregular heart rhythms. Your doctor will determine the best treatment for you and discuss the benefits and risks of these therapies with you.
- Electrical cardioversion Patients with persistent arrhythmias, such as atrial fibrillation, may not be able to achieve a normal heart rhythm with drug therapy alone. Electrical cardioversion delivers an electrical shock to your chest wall, which synchronizes the heart and allows the normal rhythm to restart. This procedure is done after you receive short-acting anesthesia.
- Catheter ablation: During ablation, energy is delivered through a catheter to tiny areas of the heart muscle. This energy can either “disconnect” the pathway of the abnormal rhythm, block the abnormal pulses and promote normal conduction of impulses, or disconnect the electrical pathway between the atria and the ventricles.
- Pulmonary vein isolation: In patients with frequent, paroxysmal or persistent atrial fibrillation, isolation of the pulmonary veins is a procedure that uses special catheters to render bands of vein tissue, thought to cause atrial fibrillation, dysfunctional. The goal is to isolate, rather than ablate, the foci responsible for triggering atrial fibrillation through a circumferential conduction block.
- Electrical devices
- Permanent pacemaker: A device that sends small electrical impulses to the heart muscle to maintain a normal heart rate. The pacemaker has a pulse generator (which houses a battery and a tiny computer) and leads (wires) that send impulses from the pulse generator to your heart muscle, as well as sense the heart’s electrical activity. Pacemakers are mostly used to prevent the heart from beating too slowly. Newer pacemakers have many sophisticated features that are designed to help manage arrhythmias, optimize heart rate-related functions and improve synchronization.
- Implantable cardioverter-defibrillator (ICD): A sophisticated electronic device used primarily to treat ventricular tachycardia and ventricular fibrillation — two life-threatening abnormal heart rhythms. The ICD constantly monitors the heart rhythm. When it detects a very fast, abnormal heart rhythm, it delivers energy to the heart muscle to cause the heart to beat in a normal rhythm again.
There are several ways an ICD can restore a normal heart rhythm:
Irregular Pulse Rate
- Antitachycardia pacing (ATP): When the heart beats too fast, a series of small electrical impulses are delivered to the heart muscle to restore a normal heart rate and rhythm.
- Cardioversion: A low-energy shock is delivered at the same time as the heartbeat to restore a normal heart rhythm.
- Defibrillation: When the heart is beating dangerously fast or irregularly, a higher energy shock is delivered to the heart muscle to restore a normal rhythm.
- Antibrachycardia pacing: Many ICDs provide back-up pacing to prevent heart rhythms that are too slow.
Heart surgery
Surgery may be needed to correct arrhythmias that can’t be controlled with medications or nonsurgical treatment methods. Arrhythmia surgery may also be recommended if you need surgery, such as valve surgery or bypass surgery, to correct other forms of heart disease. The Maze and modified Maze procedures are two surgeries used to correct atrial fibrillation.Your doctor will determine the best treatment for you and discuss these options with you, including more information about surgical treatment if it is an appropriate treatment option.
Prevention
Regular Follow-up Visits
You will need to visit your doctor for regular follow-up visits to:
- Make sure your arrhythmia is controlled
- Properly adjust your medications
- Evaluate the function of any implanted devices
- Make sure you are staying healthy and not having other medical problems
Your doctor will tell you how often you should visit. Call your doctor in between visits if your symptoms become more frequent or severe.
Resources
Doctors vary in quality due to differences in training and experience; hospitals differ in the number of services available. The more complex your medical problem, the greater these differences in quality become and the more they matter.
Clearly, the doctor and hospital that you choose for complex, specialized medical care will have a direct impact on how well you do. To help you make this choice, please review our Miller Family Heart, Vascular & Thoracic Institute Outcomes.
Cleveland Clinic Heart, Vascular & Thoracic Institute Cardiologists and Surgeons
Choosing a doctor to treat your abnormal heart rhythm depends on where you are in your diagnosis and treatment. The following Heart, Vascular & Thoracic Institute Sections and Departments treat patients with Arrhythmias:
- Section of Electrophysiology and Pacing: cardiology evaluation for medical management or electrophysiology procedures or devices - Call Cardiology Appointments at toll-free 800.223.2273, extension 4-6697 or request an appointment online.
- Department of Thoracic and Cardiovascular Surgery: surgery evaluation for surgical treatment for atrial fibrillation, epicardial lead placement, and in some cases if necessary, lead and device implantation and removal. For more information, please contact us.
- You may also use our MyConsult second opinion consultation using the Internet.
The Heart, Vascular & Thoracic Institute has specialized centers to treat certain populations of patients:
Learn more about experts who specialize in the diagnosis and treatment of arrhythmias.
For younger patients with abnormal heart rhythms:
See About Us to learn more about the Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute.
Contact
If you need more information, click here to contact us, chat online with a nurse or call the Miller Family Heart, Vascular & Thoracic Institute Resource & Information Nurse at 216.445.9288 or toll-free at 866.289.6911. We would be happy to help you.
Becoming a Patient
Treatment Options
Treatment Guides
Diagnostic Tests
Diagnostic tests are used to diagnose your abnormal heartbeat and the most effective treatment method.
Regular Irregular Pulse
Related Health Information
- Long Q-T Syndrome
Anatomy
Webchats
Our webchats and video chats give patients and visitors another opportunity to ask questions and interact with our physicians.
Videos and Podcasts
Interactive Tools
Resource Links
- Visit Health Essentials - Read articles on rhythm disorders and healthy living on Health Hub
Surgical Outcomes
Regularly Irregular Pulse
Why choose Cleveland Clinic for your care?
Irregular Pulse Interval
Our outcomes speak for themselves. Please review our facts and figures and if you have any questions don't hesitate to ask.
